Üriner İnkontinans Tedavi
Üriner inkontinans tedavisi üç kategoriye ayrılır:
1-Davranışsal tedaviler
2-Farmakoterapi
3-Cerrahi tedavi
1-Davranışsal ve Nonfarmakolojik Tedaviler:
- Sıkışma veya stres tipi inkontinans olan hastaların çoğunda tedavinin ilk aşaması davranışsal terapi olmalıdır.
- Hafif inkontinans vakalarında basit yaşam tarzı değişiklikleri yararlıdır.
- İlk basamak olarak özellikle akşamları sıvı kısıtlaması ve kafein, alkol alınmaması önerilir.
- Hasta obez ise kilo vermesi önerilir.
Mesane Eğitimi:
- Bu teknik hastaların programlı zamanlarda işeme şeklinde eğitilmeleri ile işeme reflekslerini kontrol etmelerini sağlar.
- İnkontinans tipini ve inkontinans sıklığını belirlemek için hastadan yaklaşık 1 hafta işeme kaydı tutması istenir.
Daha sonra hastanın alışılmış inkontinans aralıklarından daha kısa aralıklarla bir zamanlı işeme programı geliştirilir.
Zamanlı İşeme
- Bakıma muhtaç hastalarda pasif tuvalet yardım programıdır.
- Amaç mesane fonksiyonunu düzeltmekten çok inkontinans sıklığını önlemektir.
- Bakıcı hasta için gece dahil belirli bir zamanlı işeme programı hazırlar.
Mesane eğitiminde olduğu gibi işemeyi geciktirme veya sıkışma hissine direnme gibi girişimler yoktur
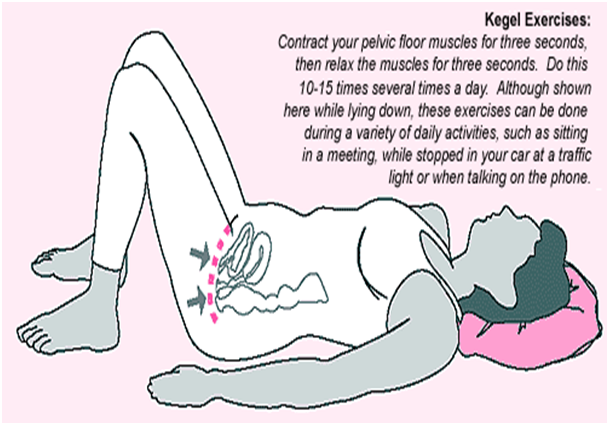
Pelvik Taban egzersizleri (Kegel egzersizleri):
- Periüretral ve perivajinal kasları kuvvetlendirmek için tasarlanmıştır.
- Stres tipi inkontinansta yararlıdır ancak sıkışma ve karışık tipteki inkontinansta da etkili olabilmektedir.
Hastalara ilk önce kaslarını nasıl kasacakları anlatılır bunun için idrarı tutmak ister gibi genital bölgedeki kaslarını sıkmaları istenir.
- Doğru kaslar tanınınca hastalara 10 saniye bu kasları kasmaları 10 saniye gevşetmeleri anlatılır.
- Bu egzersiz günde 30-80 kez tekrarlanmalıdır.
- Daha sonra hastalara inkontinansı önlemek için kaçırma anından önce ve kaçırma esnasında pelvik kaslarını kasmaları anlatılır.
2-Farmakolojik Tedavi:
Uzman hekim tarafından inkontinansın çeşidine göre verilir.En sık kullanılan ilaçlar antikolinerjikler ve trisiklik antidepresanlardır.
3-Cerrahi Tedavi:
Az şiddetli inkontinans durumlarında askı sistemleri ( TOT, TVT, MiniSling ), şiddetli inkontinans durumlarında ise yapay üriner kontrol sistemi kalıcı bir çözüm sağlamak için güvenilir yöntemlerdendir.
TOT Operasyonu: Nispeten yeni bir ameliyat yöntemidir. İlk kez 2001 yılında tarif edilmiştir. Bu ameliyatta vajinal yolla yapılan ince bir kesi ile “polipropilen mesh” adı verilen bir bant, özel bir iğne yardımı ile yerleştirilerek üretral kanal yükseltilir. TOT ameliyatında hastada yara iyileşmesi oldukça hızlı, hastanede kalış süresi oldukça az (ortalama bir gün) ve ameliyat sonrası şikayetler oldukça azdır. Ameliyattan 24 saat sonrasına kadar mesane içine yerleştirilen bir sonda ile mesanenin direne olması sağlanır. Daha sonra sonda çekilir.
TVT Operasyonu: 1995’den bu yana uygulanan bu ameliyatlar “tension-free vaginal tape” (TVT) olarak adlandırılmıştır. TVT operasyonları lokal, bölgesel veya genel anestezi eşliğinde uygulanabilir. Operasyondaki amaç üretra çevresine yerleştirilen “polipropilen bant” tan oluşan askı materyali ile üretranın yükseltilmesidir. Zaman içinde bu bant doku reaksiyonu ile nedbe yapısı oluşturarak üretraya destek sağlamaktadır. Diğer ameliyatlara göre daha az travmatik bir operasyondur.