What is Hypospadias?
Hypospadias is a congenital condition where the urethral opening is not located at the tip of the penis but rather on the underside. It is the second most common congenital anomaly in male children, occurring in about 1 in every 250 births.
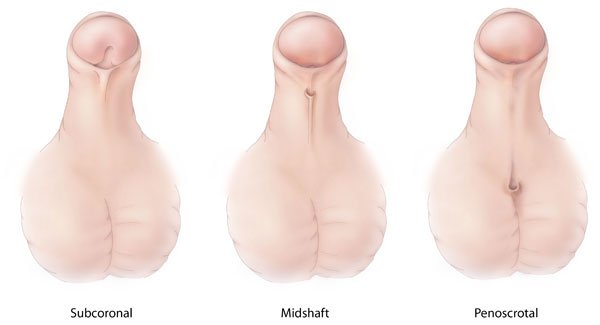
In boys with hypospadias, the urinary opening (meatus) is located below the tip of the penis. The area between this opening and the tip of the penis lacks a fully formed urethral canal. Hypospadias can be classified based on the location of the urethral opening. If the opening is near the normal location at the head of the penis, it is called glandular hypospadias. When the opening is between the head and the shaft of the penis, it is referred to as coronal hypospadias. Both of these are generally categorized as “distal hypospadias” and are the most common, with the highest success rate for surgical correction. Hypospadias can also occur lower down, with the urethral opening located anywhere along the shaft of the penis, at the junction between the penis and the scrotum, or even near the perineum close to the anus. These lower placements are more challenging to treat surgically.
Symptoms of Hypospadias
Hypospadias is often referred to colloquially with terms such as “prophet’s circumcision,” “congenital circumcision,” or “partial circumcision” because the foreskin is underdeveloped on the front side of the penis and only present on the backside.
A condition called chordee, where the penis curves during an erection, is often associated with hypospadias. The severity of chordee usually increases with the severity of hypospadias, meaning the further the urethral opening is from the tip of the penis, the more pronounced the curvature. One of the primary goals of hypospadias surgery is to correct this curvature.
Children with hypospadias may prefer to urinate while sitting because their urine stream points downward rather than forward.
Is Hypospadias Congenital? How Common is It?
Hypospadias is indeed a congenital condition, meaning it is present at birth. The exact cause is not known, but it is believed to be related to incomplete hormonal stimulation during fetal development. This theory is supported by the presence of other urogenital anomalies in severe cases of hypospadias.
It is one of the most common conditions encountered in pediatric urology, with an incidence of about 1 in every 250 male births. Distal hypospadias, where the urethral opening is near the tip of the penis, is the most frequently observed type.
A careful physical examination of a newborn can easily diagnose hypospadias.
Should Additional Tests Be Conducted After Diagnosing Hypospadias?
In cases of severe hypospadias, additional urogenital anomalies are more likely. Therefore, it is important to evaluate the urinary system (kidneys, urinary tract, and bladder) in such cases. If hypospadias is accompanied by bilateral undescended testes, chromosomal studies should be conducted to determine if there is a disorder of sexual differentiation.
When Should Treatment Be Administered?
The only treatment for hypospadias is surgical. It is best performed before the child becomes aware of their sexual identity, typically during the diaper-wearing stage, to avoid the psychological impact of penile surgery during the phallic stage (ages 2-6). Early surgery also simplifies postoperative care.
Who Should Perform Hypospadias Surgery?
There are approximately 500 different surgical techniques described for hypospadias repair. While many surgeons, including plastic surgeons, urologists, pediatric surgeons, and even general surgeons, claim expertise in this area, evidence-based literature suggests that the surgery should be performed by pediatric urology specialists or experienced pediatric surgeons to minimize complications.
What is Done During Hypospadias Surgery?
The primary goal is to reposition the urethral opening to the tip of the penis. The question of whether to use sutures or grafts depends on the specific case. Generally, a new urethral canal is created with sutures and then reinforced with a graft for added strength. Any curvature of the penis must also be corrected.
Depending on the severity of the hypospadias, circumcision may be performed simultaneously, or the foreskin may be used as a graft. Contrary to some opinions, combining hypospadias repair with circumcision can prevent the need for a second surgery.
What to Expect Post-Surgery? How Long is Hospital Stay? Is a Catheter Required?
Experienced pediatric urologists or pediatric surgeons now often perform hypospadias surgeries as outpatient procedures. The child can typically go home the same day. The dressing is removed on the third or fifth day post-surgery, and the catheter is usually removed on the seventh day. Hospitalization is not necessary.
Urinary stents are essential for healing. Babies can go home with a double-diaper technique to manage the stent. For older children, the stent is trimmed close to the glans, allowing them to urinate independently.
What are the Complications?
As mentioned earlier, the complication rate is high when surgeries are performed by inexperienced hands. Ideally, the condition should be resolved with a single surgery. The success rate of subsequent surgeries is lower if the initial surgery was unsuccessful.
The most common complication is fistula formation, where urine leaks from multiple openings due to suture breakdown. This complication cannot be addressed until six months post-surgery but is relatively easy to fix. Other complications include complete suture breakdown, bleeding, penile skin gangrene, strictures, and persistent curvature.
